Tooth decay is one of the most significant health challenges facing children today.
According to the National Institute of Dental and Craniofacial Research, nearly 46% of children in the U.S. are affected by this largely preventable condition.

As a parent, understanding the causes and consequences of tooth decay is crucial for maintaining your child's oral health.
This comprehensive guide will explore the causes, symptoms, prevention strategies, and treatment options for tooth decay in children of all ages.
Tooth decay, also known as dental caries, is a prevalent issue affecting children's oral health globally. It is a bacterial infection that causes demineralization of tooth enamel, leading to cavities.
Tooth decay occurs when bacteria in the mouth break down food, especially sugars, and produce acid, which damages the enamel of teeth. The environment starts shaping a child's oral microbiome from birth, even before teeth erupt. Primary teeth have thinner enamel than permanent teeth, making them more susceptible to decay.
Several factors contribute to children's vulnerability to tooth decay.
| Risk Factor | Description |
|---|---|
| Thinner Enamel | Children's primary (baby) teeth have thinner and less mineralized enamel. |
| Inadequate Oral Hygiene | Young children often lack the manual dexterity to properly clean their teeth. |
| Dietary Habits | Children's diets frequently contain more sugary foods and drinks. |
| This increases their risk of tooth decay. | |
Tooth decay in children is a significant public health concern that warrants attention to its prevalence. The issue is particularly pressing given the potential long-term consequences for children's oral health and overall well-being.
Tooth decay is a significant issue even among very young children. Research indicates that a substantial number of children in this age group experience tooth decay, often due to inadequate oral hygiene practices and dietary habits.
As children grow older, the prevalence of tooth decay continues to be a concern. Data suggests that children in this age group have experienced dental caries in their primary teeth, with some also beginning to experience issues with their permanent teeth.
For children aged 9-11, the statistics are particularly noteworthy. Approximately 17% of children in this age group have experienced dental caries in their permanent teeth, marking a significant transition in dental health concerns. Key statistics for this age group include:
Tooth decay in kids is primarily caused by a combination of dietary habits, oral hygiene practices, and bacterial presence. Understanding these factors is crucial for developing effective prevention strategies.
A diet high in sugars significantly contributes to tooth decay in children. When bacteria in the mouth feed on sugars, they produce acids that damage tooth enamel, leading to caries.
Inadequate brushing and flossing allow plaque to build up on tooth surfaces, fostering an environment where bacteria thrive. Regular oral hygiene practices are essential to prevent the onset of decay.
Bacteria, particularly Streptococcus mutans and Lactobacillus, play a crucial role in initiating caries. These bacteria are transmitted to children through close contact with caregivers. Research has shown that mothers with active caries can transmit decay-causing bacteria to their child, highlighting the importance of maternal oral health.

Recognizing the signs and symptoms of tooth decay is vital for ensuring the oral health of children. Tooth decay can progress without noticeable symptoms until it's advanced, making regular checks crucial.
Early detection of tooth decay can significantly improve treatment outcomes for children. Some early warning signs include initial changes in tooth color or sensitivity. Parents should be vigilant about any changes in their child's teeth and report them to a dentist.
Advanced tooth decay can lead to severe consequences, including pain and infection. If a child exhibits any of the following symptoms, parents should seek immediate dental care.
The impact of untreated tooth decay in children extends beyond oral health, influencing their physical and emotional well-being. When decay is left untreated, it can lead to a range of serious health issues.
Untreated tooth decay can result in chronic pain and discomfort for children, significantly affecting their quality of life. In severe cases, the infection can spread, potentially leading to more serious health complications, including the risk of bacteria traveling to the brain.
Children with visible tooth decay often face social stigma and bullying, which can lead to decreased self-esteem and social withdrawal. Furthermore, premature tooth loss due to decay can impair speech development, as certain sounds require specific tooth positions to be properly articulated. The overall condition can also impact school performance and psychological well-being.
Effective prevention strategies are crucial in maintaining good oral health in children and reducing the incidence of tooth decay.
Several key practices can help prevent tooth decay in children. These include proper brushing and flossing techniques, the use of fluoride, dietary recommendations, and regular dental check-ups.
Teaching children proper brushing and flossing techniques is essential for removing plaque and bacteria that cause decay. Parents should supervise their child until they are old enough to perform these tasks effectively on their own.
Fluoride plays a critical role in preventing tooth decay by making teeth more resistant to acid attacks from plaque bacteria and sugars in the mouth. Regular application of fluoride through toothpaste and professional treatments can significantly enhance oral health.
A healthy diet is crucial for maintaining good health and preventing tooth decay. Limiting sugary snacks and drinks, and encouraging the consumption of fruits, vegetables, and dairy products can help.
Regular visits to a dentist are vital for maintaining good oral health. The American Academy of Pediatric Dentistry recommends that children have their first dental visit by their first birthday or within six months after their first tooth erupts. Regular check-ups every six months allow for early detection of decay, professional cleanings, and preventive treatments like sealants and fluoride applications.
By implementing these strategies, parents can help their children maintain good oral health and reduce the risk of tooth decay. Regular consultations with a dentist can provide personalized guidance tailored to each child's needs.

The treatment of tooth decay in children involves a range of approaches, from preventive measures to more invasive procedures. The choice of treatment depends on the extent and severity of the decay, as well as the child's overall health and age.
For early stages of tooth decay, fillings and restorations are common treatments. These procedures involve removing the decayed portion of the tooth and filling it with a suitable material, such as composite resin or amalgam, to restore the tooth's function and appearance.
Silver Diamine Fluoride (SDF) treatment is a non-invasive option used to arrest the progression of tooth decay. SDF is applied directly to the affected tooth, helping to prevent further decay and potentially avoiding the need for more invasive treatments.
In cases where decay has reached the pulp of the tooth, pulp therapy may be necessary to save the tooth. If the tooth is beyond saving, extraction may be required. These procedures are typically performed by a pediatric dentist.
For very young children or those with extensive decay, general anesthesia may be recommended to facilitate treatment. This decision is made carefully, considering the risks and benefits, and is typically carried out in a hospital setting.
Understanding these treatment options can help parents make informed decisions about their child's dental care, ensuring they receive the most appropriate treatment for their specific needs.
Tooth decay and other oral health issues disproportionately affect certain groups of children, highlighting the need for targeted interventions. Research supported by the National Institute of Dental and Craniofacial Research (NIDCR) is focused on understanding and addressing these disparities.
Socioeconomic status significantly influences children's oral health. Children from low-income families are more likely to experience tooth decay due to limited access to dental care, unhealthy dietary habits, and inadequate oral hygiene practices. Effective strategies are needed to reach these vulnerable populations.
Racial and ethnic disparities in children's oral health are pronounced, with certain minority groups experiencing higher rates of tooth decay. Cultural and linguistic barriers can hinder access to care, making it essential to develop culturally sensitive interventions. Community-based programs have shown promise in addressing these disparities.
Improving access to dental care is critical for reducing disparities in children's oral health. Innovative solutions such as school-based dental programs, teledentistry, and mobile dental clinics are expanding care options. The following table highlights some effective strategies:
| Strategy | Description | Impact |
|---|---|---|
| School-based dental programs | Provide preventive services like sealants and fluoride treatments | Increased access to care for underserved children |
| Teledentistry and mobile clinics | Bring services directly to underserved communities | Reduced transportation barriers and increased care options |
| Integration of oral health into primary care | Allow for dental screenings and referrals during well-child visits | Early detection and intervention for oral health issues |
A healthy mouth in children lays the foundation for a lifetime of oral and overall health. As emphasized by NIDCR Director Rena D'Souza, "Scientific and technological advances in recent decades have significantly expanded our ability to prevent and treat dental caries."
To help prevent tooth decay, parents should focus on establishing good oral hygiene habits early in life. This includes proper home care, regular dental visits, a tooth-friendly diet, and the appropriate use of fluoride products.
By following these tips and staying committed to good oral health practices, parents can help their children maintain a healthy smile for life.
The primary cause of cavities, also known as caries, in young children is the frequent consumption of sugary drinks and foods, combined with poor oral hygiene habits. Bacteria in the mouth feed on sugars and produce acid, which damages the enamel and leads to cavities.
To help prevent cavities, encourage your child to practice good oral hygiene habits, such as brushing their teeth with fluoride toothpaste at least twice a day and visiting the dentist regularly. Limit sugary drinks and foods, and consider using a water bottle instead of a bottle with juice or milk.
Fluoride plays a crucial role in preventing tooth decay by making the teeth more resistant to acid attacks from bacteria. It can be applied topically through toothpaste, mouthwashes, or professional treatments at the dentist.
The American Academy of Pediatric Dentistry recommends that children visit the dentist by their first birthday or within six months of the eruption of their first tooth. Regular dental check-ups can help identify oral health issues early on and prevent more serious problems.
Yes, putting a child to bed with a bottle containing milk, juice, or other sugary drinks can contribute to tooth decay. The sugars in these liquids can pool around the teeth, creating an ideal environment for bacteria to thrive.
To manage sensitivity after a dental treatment, your child can use a desensitizing toothpaste or avoid eating or drinking extreme temperatures. If the sensitivity persists, consult with your child's dentist for further guidance.
The quest for a straighter smile has led to a significant rise in the popularity of clear aligners as a preferred alternative to traditional braces.
As orthodontic treatment options continue to evolve, many potential patients are left wondering: are aligners effective for teeth straightening?

The effectiveness of aligner treatment depends on several key factors, which we will explore in this article.
We will delve into the science behind aligners, their advantages, and disadvantages, as well as who they're best suited for.
The advent of clear aligners has transformed the landscape of orthodontics, providing a nearly invisible treatment option. Clear aligners are transparent, custom-made trays that fit over your teeth to gently guide them into the desired position.
Orthodontic treatment has evolved significantly over the years, from traditional metal braces to the development of clear aligners in the late 1990s. Invisalign was the pioneer in this field, and the expiration of key patents in 2017 led to the proliferation of various clear aligner brands and options.
Today, there are several types of clear aligners available, including in-office options supervised by dentists/orthodontists and direct-to-consumer alternatives. The materials used in modern clear aligners have improved over time, becoming more effective and comfortable.
| Type of Aligner | Supervision | Cost |
|---|---|---|
| In-office Aligners | Dentist/Orthodontist | Moderate to High |
| Direct-to-consumer Aligners | Limited or Remote | Low to Moderate |
convenient and aesthetically pleasing solution for individuals seeking to straighten their teeth without the use of traditional metal braces. With various options available, it's essential to consult with an orthodontic professional to determine the best course of treatment.
Aligners work by leveraging the body's natural ability to remodel bone in response to applied forces. This process is fundamental to understanding how clear aligners can effectively move teeth into a better alignment.
The science behind aligners involves applying gentle, controlled force to teeth in specific directions. This force stimulates bone remodeling, a natural process where the bone is broken down on one side of the tooth and rebuilt on the other, supporting the tooth's new position. The application of pressure at specific points is crucial for this process.
The clear aligner process begins with an initial consultation and 3D scanning, followed by treatment planning and the manufacturing of custom aligners. Digital technology maps out the entire tooth movement journey before treatment begins. Patients wear each set of aligners for a specified period, typically 20-22 hours a day, and progress through multiple sets over the course of treatment.
| Step | Description |
|---|---|
| Initial Consultation | Assessment of suitability for clear aligner treatment |
| 3D Scanning | Creation of a digital model of the patient's teeth |
| Treatment Planning | Mapping out the tooth movement journey |
| Manufacturing | Production of custom aligners based on the treatment plan |

Recent studies have shed light on the efficacy of clear aligners in treating various orthodontic issues. Clear aligners have become a popular choice for teeth straightening due to their aesthetic appeal and convenience.
A 2023 review by Consumer Affairs found that clear aligner therapy works for mild to moderate tooth movements 80% to 90% of the time. This impressive success rate makes clear aligners a viable option for many patients. Clinical studies have consistently shown that clear aligners are effective in treating mild to moderate misalignments.
The success of clear aligner treatment is influenced by several factors, including patient compliance and the complexity of the dental issue. Patients are required to wear aligners for 20-22 hours daily, and adherence to this regimen significantly impacts treatment outcomes. The complexity of the case also plays a crucial role, with mild to moderate cases showing the highest success rates.
| Treatment Outcome | Success Rate | Factors Influencing Success |
|---|---|---|
| Mild to Moderate Misalignments | 80-90% | Patient Compliance, Complexity of Case |
| Complex Orthodontic Issues | Lower than 80% | Severity of Misalignment, Patient Compliance |
Over the years, clear aligners have evolved to correct a wide range of dental problems. They are now used to treat various dental issues, including misalignments, overcrowding, gaps between teeth, and bite issues.
Clear aligners are particularly effective in treating mild to moderate misalignments. They work by gradually shifting teeth into proper alignment, resulting in a straighter smile.
Overcrowding occurs when there's insufficient space in the jaw for all teeth, causing them to overlap. Aligners address this by creating space and shifting teeth into proper alignment. Gaps between teeth, or diastemas, can be closed by applying consistent pressure to guide teeth together.
Various bite issues, including overbites, underbites, crossbites, and open bites, can be treated with clear aligners. These issues are addressed by adjusting the position of teeth to achieve a proper bite.
While clear aligners are effective for many dental issues, they have limitations. Severe orthodontic cases involving significant jaw misalignment or complex tooth rotations may require additional treatments.
| Dental Issue | Treatment Capability |
|---|---|
| Mild to Moderate Misalignments | Effective |
| Overcrowding and Gaps | Effective |
| Bite Issues | Effective for various bite issues |
| Severe Misalignments | Limited |

While clear aligners offer numerous benefits, they also have some drawbacks that need to be considered.
One of the main disadvantages is the cost. Clear aligner treatment can be more expensive than traditional braces, with prices ranging from $3,000 to $8,000 depending on the complexity of the case.
The cost of clear aligners can be a significant factor for many patients. Many dentists offer interest-free credit to help spread the cost of treatment, making it more manageable.
Clear aligners require a high level of discipline, as they need to be worn for around 22 hours per day. Failure to comply with this requirement can lead to extended treatment time and suboptimal results.
Clear aligners are not suitable for all orthodontic cases, particularly complex ones involving severe rotations or significant bite corrections. In such cases, traditional braces may be a better option or choice.
Understanding the clear aligner treatment process is crucial for achieving the desired orthodontic results. The journey begins with a comprehensive initial consultation.
The process starts with a consultation with a dentist or orthodontist who evaluates your suitability for clear aligner treatment. This phase involves digital scanning and treatment planning using 3D imaging technology to create a virtual model of your teeth and project the step-by-step movement to the desired final position.
You will receive a full case of numbered aligners at the start of your treatment plan. It's essential to wear the aligners for 22 hours a day and change them every 10-14 days as outlined in your plan. Proper maintenance includes cleaning and storing them appropriately when not in use.
Regular check-ups with your dentist or orthodontist are crucial to ensure your teeth are moving as planned. Mid-treatment adjustments may be necessary, and refinements with additional aligners can be made to achieve optimal results.
| Treatment Stage | Description | Duration |
|---|---|---|
| Initial Consultation | Evaluation and planning | 1 visit |
| Wearing Aligners | Daily wear and maintenance | Ongoing |
| Monitoring Progress | Regular check-ups | Every 4-6 weeks |
Determining whether clear aligners are the right choice for a patient involves considering several key factors, including the type and severity of their dental issues.
Clear aligners are most effective for patients with mild to moderate dental misalignments, including issues such as minor crowding, spacing problems, and certain bite corrections. Adults and teens who are committed to following the treatment protocol are ideal candidates.
In cases requiring significant tooth rotation, vertical movement of teeth, or major bite corrections, traditional braces might be a more suitable option. An experienced orthodontist can help determine the best treatment choice based on individual needs.
In conclusion, clear aligners present a modern orthodontic treatment option that is both effective and discreet. By understanding how clear aligners work and their effectiveness for various dental issues, individuals can make an informed decision about their smile.
It's crucial to consult with a qualified dentist to determine if clear aligners are the right choice for your needs. They can help create a personalized treatment plan that suits your lifestyle and goals, ensuring a healthier, more confident smile and properly aligned teeth.
Clear aligners are made of a BPA-free plastic material that is custom-made to fit your teeth. The plastic is durable and resistant to wear, ensuring that the aligners remain effective throughout the treatment process.
The length of treatment varies depending on the individual's dental issues and the complexity of the case. On average, treatment can last anywhere from a few months to a few years, with some cases requiring 12 to 18 months of treatment.
For optimal results, clear aligners should be worn for 20 to 22 hours a day. This allows for consistent pressure on the teeth, guiding them into the desired position.
Yes, clear aligners can be used to treat mild to moderate bite issues, such as overbites and underbites. However, more complex bite issues may require traditional orthodontic treatment.
Clear aligners are ideal for individuals with mild to moderate misalignments. Those with more complex dental issues may require traditional orthodontic treatment, such as braces.
The cost of clear aligners varies depending on the provider, the complexity of the case, and the location. On average, the cost can range from ,000 to ,000.
It is recommended to remove your clear aligners when eating and drinking to prevent damage and staining. You can drink water with your aligners in, but it's best to avoid consuming other beverages.
Regular check-ups with your orthodontist are necessary to monitor progress and make any necessary adjustments to your treatment plan. The frequency of visits will depend on your individual treatment plan.
Choosing between braces and aligners can be a daunting task, especially with the numerous options available for orthodontic treatment. Many patients struggle to decide which option is best for their specific dental needs and lifestyle preferences.
The decision to opt for orthodontic treatment is a significant one, and it's essential to consider the various factors involved. Modern orthodontic treatment offers multiple options for straightening teeth and correcting bite issues.

Both braces and aligners are effective in moving teeth into proper alignment, but they differ in appearance, comfort, and maintenance requirements. Understanding these differences is crucial in making an informed decision about which treatment option will best suit your needs and personal preferences.
When considering orthodontic treatment, understanding the available options is crucial. Orthodontic treatments have evolved significantly, offering a range of choices tailored to individual needs and preferences.
Traditional braces are a well-established orthodontic treatment. They consist of metal brackets bonded to the teeth and connected by wires and rubber bands, which apply gentle pressure to guide the teeth into the correct position.
Modern metal braces are more comfortable and less noticeable than their predecessors. They remain the most effective solution for complex orthodontic issues, including severe crowding and significant bite problems.
| Feature | Description |
|---|---|
| Brackets | Made of metal, bonded to teeth |
| Wires | Apply gentle pressure to move teeth |
| Rubber Bands | Used to adjust the force on the teeth |
Clear aligners are a popular alternative to traditional braces, especially among adults and teenagers concerned about aesthetics. Made from plastic, these custom-made trays are designed to fit snugly over the teeth, gradually shifting them into the desired position.
Each set of clear aligners is worn for a specified period before being replaced by the next set in the series, with the treatment plan digitally mapped out beforehand. For complex movements, small tooth-colored attachments may be used to help the aligners grip the teeth more effectively.

Understanding the differences between braces and aligners is crucial for making an informed decision. When considering orthodontic treatment, several factors come into play, including appearance, comfort, treatment time, and convenience.
The appearance of orthodontic appliances is a significant concern for many patients. Clear aligners are less noticeable than traditional braces as they are custom-made to fit your teeth. This makes them an attractive option for adults and professionals who are concerned about their appearance during treatment.

Comfort is another critical factor to consider. Generally, aligners are more comfortable than braces because they are smoother and cause less irritation to the lips and cheeks. However, some discomfort may be experienced when switching to a new set of aligners.
The treatment time varies depending on the complexity of the case. Metal braces often work faster for complex cases because they can provide more force to move teeth quickly. On average, treatment with braces can take 12-24 months, while clear aligners may take 6-18 months.
The removability of aligners is a significant advantage. They can be removed for eating, drinking, and cleaning, making oral hygiene easier to maintain. However, this requires patients to be disciplined and wear the aligners for the recommended 20-22 hours per day.
Understanding the day-to-day implications of braces versus clear aligners is crucial for making an informed decision. The practical aspects of orthodontic treatment can significantly influence a patient's choice between these two options.
Maintaining good oral hygiene is significantly easier with clear aligners since they are removable, allowing patients to brush and floss normally. In contrast, braces require special brushes and flossing tools to clean around brackets and under wires, which can be time-consuming and may lead to plaque buildup if not done properly.
Clear aligners offer complete dietary freedom since they are removed before eating, allowing patients to enjoy their favorite foods without restrictions. On the other hand, patients with braces must avoid hard, sticky, and crunchy foods that could damage brackets or wires, such as popcorn, nuts, and hard candies.
The frequency and duration of follow-up visits differ between the two treatment options. Braces typically require monthly adjustments that take longer to complete, whereas aligner patients generally have less frequent check-ups (every 6-8 weeks) and shorter appointments.
| Practical Aspect | Braces | Clear Aligners |
|---|---|---|
| Oral Hygiene | More challenging; requires special tools | Easier; removable for normal brushing and flossing |
| Dietary Restrictions | Must avoid hard, sticky, and crunchy foods | No restrictions; removable before eating |
| Follow-up Appointments | Monthly adjustments; longer appointments | Less frequent (every 6-8 weeks); shorter appointments |
The practical aspects of daily life with orthodontic treatment often become the deciding factor for many patients when choosing between braces and aligners. By considering these factors, patients can make a more informed decision that suits their lifestyle.
Understanding the cost and insurance considerations for orthodontic treatment can help patients make informed decisions. The cost of orthodontic care varies widely depending on several factors, including the complexity of the case, geographic location, and the orthodontist's experience.
The cost of metal braces typically ranges from $3,000 to $7,000 for a full treatment course. Factors such as case complexity and treatment duration can affect the final price. Ceramic braces, which are less visible, generally cost between $4,000 and $8,000.
Clear aligners, such as Invisalign, usually cost between $4,000 and $7,400 for full treatment. However, minor corrections may require fewer aligners, reducing the overall cost. The price for clear aligners can vary based on the treatment's complexity.
Many dental insurance plans offer orthodontic coverage, typically covering 25% to 50% of the total cost up to a lifetime maximum. Patients should verify their insurance coverage before beginning treatment. Most orthodontic practices offer flexible payment plans, and patients can also use Health Savings Accounts (HSAs) and Flexible Spending Accounts (FSAs) to pay for treatment with pre-tax dollars.
When it comes to orthodontic treatment, understanding the differences between metal braces and clear aligners is crucial. The decision between these two orthodontic treatment options depends on several factors, including the complexity of your case, personal preferences, and budget.
For patients with complex orthodontic issues, traditional braces may offer the most effective solution. On the other hand, clear aligners are ideal for those with mild to moderate alignment issues who value aesthetics and convenience. It's essential to consider your daily routine and lifestyle when making your decision.
Consulting with an experienced orthodontist is key to determining the best treatment option for your specific needs. They can provide personalized recommendations and help you understand the implications of each choice on your day-to-day life. Remember, the goal of treatment is not just to align your teeth but to enhance your overall smile and confidence.
Ultimately, the most successful orthodontic treatment is one that fits seamlessly into your life. By carefully considering your options and following your orthodontist's guidance, you can achieve the best possible outcome for your teeth and overall oral health.
The primary difference lies in their appearance and material. Metal braces are fixed and consist of metal brackets and wires, whereas clear aligners are removable, made of plastic, and nearly invisible.
To maintain good oral hygiene, it's essential to brush and floss regularly, especially after meals. With clear aligners, you can remove them to clean your teeth, while with metal braces, you'll need to use a proxy brush to clean around the brackets.
Yes, certain foods can damage your orthodontic appliances. With metal braces, it's best to avoid hard, sticky, or chewy foods like popcorn, nuts, or caramels. With clear aligners, you can remove them while eating, but it's still crucial to maintain good oral hygiene.
The frequency of visits depends on the type of orthodontic treatment. For metal braces, you'll typically need to visit every 4-6 weeks for adjustments. For clear aligners, you'll need to visit every 6-8 weeks to receive new aligners.
Yes, your lifestyle can play a significant role in choosing between traditional braces and clear aligners. If you have a busy schedule or prefer a more discreet treatment option, clear aligners might be the better choice.
Insurance coverage varies depending on your provider and policy. Some plans may cover a portion of the cost, while others may not. It's essential to check with your insurance provider to understand your coverage and any out-of-pocket expenses.
A tooth can become damaged or discolored due to various reasons, affecting the overall appearance of one's smile. Fortunately, cosmetic dentistry offers a solution to repair and enhance the appearance of teeth.
Dental bonding is a popular procedure where a dentist applies a tooth-colored composite resin to one or more teeth to repair damage or improve their appearance. This cost-effective solution is considerably less expensive than other cosmetic dental procedures.

The bonding process can address multiple issues, including chips, cracks, gaps between teeth, and discoloration, significantly improving a person's smile and confidence with minimal invasiveness.

Learn More
Dental bonding is a non-invasive procedure used to restore or enhance the aesthetic appeal of teeth. It involves the application of a tooth-colored resin material that is hardened with a special light, effectively "bonding" the material to the tooth to improve or restore a person's smile.
Dental bonding is defined as a cosmetic dental procedure where tooth-colored composite resin is applied to teeth and hardened with a special light to bond the material to the tooth structure. The fundamental concept behind bonding is using adhesive materials to repair or enhance the appearance of teeth without removing significant tooth structure.
Dental bonding serves both cosmetic and restorative purposes in modern cosmetic dentistry. Unlike other cosmetic dental procedures such as veneers or crowns, dental bonding typically requires less tooth preparation, making it a more conservative treatment option. It can often be completed in a single visit to the dentist, and is generally less expensive than alternatives, making it an accessible option for many patients.
Understanding the dental bonding process is essential for patients looking to improve the aesthetic appeal of their smile. This procedure involves several key steps and materials that work together to achieve the desired outcome.
The primary material used in dental bonding is composite resin, a tooth-colored substance that mimics the appearance of natural tooth enamel. This resin is composed of a mixture of plastic and glass, providing durability and a natural look. The composite resin is available in various shades, allowing dentists to match it to the color of the patient's natural teeth.

The dental bonding procedure begins with the dentist selecting a composite resin color that closely matches the patient's natural teeth using a shade guide. The surface of the tooth is then roughened, and a conditioning liquid is applied to help the bonding material adhere. The composite resin is applied over the liquid, molded or shaped to achieve the desired form, and then hardened with an ultraviolet light. If necessary, the dentist can further shape the tooth after the resin hardens to ensure a natural appearance.
Most dental bonding procedures can be completed in a single visit, typically taking between 30 to 60 minutes per tooth. Generally, dental bonding does not require anesthesia unless it is being used to fill a cavity or if the tooth is near a nerve. This makes it a convenient option for patients with busy schedules.

Learn More
The applications of dental bonding are diverse, including both functional and aesthetic improvements. Dental bonding is a versatile and effective solution for various dental issues, making it a popular choice among patients.
Dental bonding effectively repairs damaged teeth, including chips, cracks, and fractures, restoring both function and appearance. It can fix broken teeth or tooth damage from trauma, providing a durable and aesthetic solution. This procedure is particularly useful for addressing minor to moderate damage.
Dental bonding offers several cosmetic applications, including correcting tooth discoloration that doesn't respond to whitening, reshaping irregular teeth, and lengthening teeth that appear too short. It can also close small gaps between teeth (diastemas) without the need for orthodontic treatment, enhancing the overall appearance of the smile.
Tooth-colored bonding materials can be used as an alternative to silver amalgam fillings for treating cavities, offering both functional restoration and aesthetic benefits. Additionally, dental bonding can protect exposed tooth roots resulting from gum recession, reducing sensitivity and preventing further damage.
Dentists may recommend dental bonding to address multiple cosmetic concerns simultaneously, creating a comprehensive smile makeover. This approach allows patients to achieve their desired smile with a relatively simple and non-invasive procedure.
Dental bonding offers several benefits that make it an attractive option for patients. It is a versatile and efficient cosmetic dentistry procedure that addresses various dental issues.
Dental bonding is recognized for its cost-effectiveness compared to other cosmetic dentistry services like veneers and crowns. The typical cost ranges from $100 to $400 per tooth, making it an affordable entry point for patients concerned about budget constraints. This affordability is a significant advantage, especially for those who need to repair or improve multiple teeth.
| Procedure | Typical Cost per Tooth |
|---|---|
| Dental Bonding | $100-$400 |
| Veneers | $500-$1,500 |
| Crowns | $800-$1,500 |
The conservative nature of dental bonding is another significant benefit. It requires minimal to no removal of healthy tooth structure, preserving more of the patient's natural teeth. This approach not only maintains the integrity of the tooth but also makes the procedure reversible in many cases, unlike more invasive procedures.
"Dental bonding is a conservative approach that preserves the natural tooth structure, making it a preferred option for many patients."
The convenience of completing dental bonding in a single dental visit is a notable advantage. The procedure typically takes 30-60 minutes per tooth, and most dental bonding procedures don't require anesthesia, eliminating recovery time and allowing patients to immediately return to normal activities. Additionally, dental bonding can be easily repaired or touched up if damaged, providing ongoing flexibility for maintaining the restoration.

Understanding the limitations of dental bonding is crucial for managing expectations. While it is a versatile and effective cosmetic dentistry solution, there are certain factors to consider before undergoing the procedure.
The bonding material used in tooth bonding does not last as long as other restorations like crowns or veneers. Typically, dental bonding lasts between 3 to 10 years before needing replacement. Moreover, the bonding material is not as strong as natural teeth, making it more susceptible to chipping or breaking, especially with certain habits like nail biting or ice chewing.
The resin used in dental bonding is more prone to staining than natural teeth or porcelain restorations. Common culprits include coffee, tea, tobacco, and red wine. Over time, the color stability of the bonding material may change, potentially requiring touch-ups to maintain the aesthetic appearance.
Dental bonding may not be suitable for extensive damage, large cavities, or areas with heavy bite forces. Patients with severe discoloration or significant structural issues may may need alternative treatments like veneers, crowns, or dental implants. Additionally, dentists may also recommend alternative treatments for patients with certain habits that could damage the bonding material.
Discussing expectations and limitations with your dentist is essential to determine if dental bonding is appropriate for your specific situation.
Maintaining good oral hygiene is key to keeping your bonded teeth in excellent condition. Proper care helps extend the life of the bonding material and keeps your natural teeth healthy.
To keep your bonded teeth in good condition, it's essential to follow a rigorous daily maintenance routine. This includes brushing your teeth at least twice a day with a non-abrasive toothpaste and flossing daily to remove any food particles that may get stuck between your teeth.
Using a gentle brushing technique and a soft-bristled toothbrush can help prevent damage to the bonding material. Additionally, scheduling regular professional dental cleanings every six months can help monitor the condition of your bonded teeth and address any issues early.
Certain habits can compromise the integrity of your bonded teeth. It's advisable to avoid biting your fingernails, chewing on pens or ice, and opening packages with your teeth, as these actions can cause the bonding material to chip or break.
Consuming staining substances like coffee, tea, red wine, and tobacco should also be avoided, particularly in the first 48 hours after the procedure, when the bonding material is most susceptible to stains. If you notice any chips, rough edges, or unusual sensations with your bonded teeth, contact your dentist immediately.
As a versatile treatment, dental bonding addresses various dental concerns with minimal invasion. Composite resin bonding is a highly effective cosmetic dentistry procedure for enhancing smiles by repairing tooth damage. It offers an affordable, minimally invasive option compared to more extensive treatments like dental implants.
While dental bonding has limitations in durability and stain resistance, proper care can significantly extend its lifespan. Patients should consult with their dentist to determine if dental bonding is the right choice for their specific oral health needs and cosmetic goals.
Tooth bonding is used to repair damaged teeth, improve the appearance of teeth, and fill cavities. It involves applying a composite resin material to the tooth surface.
The procedure typically requires a single visit to the dentist and can take anywhere from 30 minutes to an hour per tooth, depending on the complexity of the case.
Generally, dental bonding is not painful, and most patients do not require anesthesia. However, if the bonding is being used to fill a decay or repair a broken tooth, some discomfort may be experienced.
To maintain bonded teeth, practice good oral hygiene by brushing and flossing regularly, and avoid habits like chewing on ice or biting your nails.
Bonded teeth cannot be whitened in the same way as natural teeth. If you want to whiten your teeth, it's best to do so before undergoing tooth bonding.
With proper care, dental bonding can last for several years. However, it may need to be replaced or repaired over time due to wear and tear or staining.
Yes, tooth bonding can be used to close gaps between teeth and improve the overall appearance of your smile.
Dental bonding can be a more conservative and cost-effective alternative to veneers or crowns in some cases. However, it may not be suitable for more extensive repairs or cosmetic improvements.
A beautiful, natural-looking smile can enhance a person's overall appearance and confidence. Smile design is a comprehensive approach to creating a smile that is both aesthetically pleasing and functional.

The goal of smile design is to create a harmonious balance between a person's facial features, skin tone, and tooth color. By considering these factors, a dentist can help patients achieve a smile that not only looks great but also contributes to their overall oral health and well-being.
A comprehensive smile design involves a thorough understanding of dental health and aesthetics. It is a personalized dental approach that combines aesthetic principles with functional dental care to create harmonious, natural-looking smiles tailored to each individual.
Smile design is a tailored approach to dental care that focuses on creating a balanced and attractive smile. One of the first steps in smile design is to conduct a thorough dental examination to determine the health of the teeth and gums. This examination includes taking measurements and making molds of the teeth to understand the person's bite and tooth shape.
The science behind smile design incorporates dental anatomy, biomechanics, and oral health principles to ensure aesthetic improvements support proper function and longevity. Dentists apply artistic principles including symmetry, proportion, and color theory to create balanced smiles.
| Key Factors | Description |
|---|---|
| Facial Proportions | Analyzing the overall facial structure to ensure harmony. |
| Lip Line and Gum Display | Assessing the lip line and gum display to achieve a natural look. |
| Tooth Size, Shape, and Color | Tailoring teeth to match the individual's facial features and preferences. |
The ideal candidates for smile design are those looking to address various cosmetic and functional dental issues. Smile design can greatly improve a person's self-confidence and overall appearance, leading to life-changing results that impact both personal and professional aspects of their life.

Individuals with visible cosmetic dental concerns such as discoloration, gaps, chips, cracks, misalignment, or disproportionate teeth are ideal candidates. These issues can significantly affect their willingness to smile, making smile design a viable solution to enhance their dental health and aesthetics.
Those who feel self-conscious about their smile and often hide their teeth in photos or social situations can greatly benefit from smile design treatments. By addressing their cosmetic dentistry needs, individuals can experience a significant boost in confidence, leading to a more fulfilling personal and professional life.
Patients with functional dental issues like bite problems, worn teeth, or difficulty chewing may require smile design that addresses both aesthetic and practical concerns. By doing so, smile design can improve not only the appearance of their smile but also their overall oral health and dental health.
By understanding the needs of different individuals, a qualified cosmetic dentist can tailor a smile design treatment plan that meets their unique requirements, ultimately leading to a perfect smile that enhances their overall quality of life.
A well-planned smile design process is essential for achieving the desired outcome, and here's what you can expect. The process is tailored to each individual's needs and goals, ensuring a personalized approach to enhancing one's smile.
The smile design process typically begins with a comprehensive consultation where the dentist evaluates the patient's current smile, discusses their goals, and assesses their oral health status. During this initial assessment, detailed measurements and photographs are taken to identify any underlying issues.
Digital imaging technology plays a crucial role in modern smile design, allowing patients to preview potential results through computer simulations before committing to treatment. The treatment planning phase involves creating a detailed roadmap that outlines all procedures needed, their sequence, timeline, and how they work together to achieve the desired outcome.
The implementation phase may involve multiple appointments spread over weeks or months depending on the complexity of the case and the procedures required. Throughout the process, temporary restorations may be used to test the new smile design in real-world conditions, allowing for adjustments before final implementation.
"A successful smile design is not just about aesthetics; it's also about ensuring the long-term health and functionality of the patient's smile."
This quote highlights the importance of a comprehensive approach tosmile design.
Smile design is a personalized approach that incorporates various cosmetic dental treatments to improve the overall appearance of the teeth and smile. Several common procedures are used to achieve the desired aesthetic results.
Teeth whitening is a popular procedure that brightens the teeth, removing surface stains and yellowing. Cosmetic bonding uses tooth-colored composite resin to repair minor imperfections like chips or small gaps, offering an affordable and minimally invasive option.
Veneers are thin, custom-made shells that cover the front surface of teeth to correct multiple aesthetic issues. Crowns restore damaged teeth while improving their appearance, shape, and alignment within the smile.
Orthodontic treatments, including clear aligners and less visible braces, offer discreet options for correcting misalignment without compromising aesthetics during treatment.
Gum contouring addresses the soft tissue frame around the teeth, creating proper proportions and symmetry essential to an aesthetically pleasing smile design.
| Procedure | Description | Benefits |
|---|---|---|
| Teeth Whitening | Brightens teeth by removing stains | Immediate improvement in smile appearance |
| Veneers | Corrects aesthetic issues with thin shells | Corrects chips, cracks, gaps, and discoloration |
| Orthodontic Treatments | Corrects misalignment | Discreet options available |

"A beautiful smile can be achieved through a combination of cosmetic dental procedures tailored to individual needs."
A well-designed smile can significantly enhance one's quality of life, offering a range of aesthetic, psychological, and health-related advantages. With the help of a cosmetic dentist, patients can achieve a beautiful and functional smile that not only boosts confidence but also improves overall oral health.
The aesthetic benefits of smile design extend beyond just having straighter or whiter teeth, creating harmony between the smile and facial features that enhances overall appearance. This, in turn, can lead to significant improvements in self-confidence and positive social interactions, impacting personal and professional relationships.
From a health perspective, smile design often improves oral function, bite alignment, and makes teeth easier to clean, potentially reducing the risk of future dental problems. Properly designed and implemented dental work can provide long-term stability and durability, making smile design a worthwhile investment in both appearance and oral health.
Financial considerations include understanding the initial investment, insurance coverage limitations for cosmetic procedures, and financing options that can make smile design more accessible. Patients should carefully weigh immediate results against long-term maintenance requirements and the potential need for replacement or touch-ups of certain treatments over time.
| Benefits | Description | Impact |
|---|---|---|
| Aesthetic | Enhances overall appearance by creating harmony between the smile and facial features | Boosts confidence and improves social interactions |
| Psychological | Improves self-confidence and overall mental well-being | Positive impact on personal and professional relationships |
| Oral Health | Improves oral function, bite alignment, and makes teeth easier to clean | Reduces the risk of future dental problems and improves overall oral health |
The journey to your perfect smile begins with understanding if smile design is tailored to your needs. To make this determination, honestly assess your dental concerns, aesthetic goals, and oral health status. Consulting with experienced cosmetic dentists who specialize in smile design is crucial. They will help you understand what can be realistically achieved. Consider scheduling consultations with several dentists to compare approaches and treatment plans.
If you're ready to transform your smile and boost your confidence, schedule a smile design consultation today. At Pinecrest Dental, cosmetic dentistry and smile design dentistry merge to help you achieve a perfect blend of health and beauty.
The first step is to schedule an initial consultation with a cosmetic dentist to assess your oral health and discuss your aesthetic goals.
A dentist uses a combination of digital imaging and a thorough examination of your teeth, gums, and overall facial features to create a personalized treatment plan.
Common procedures include teeth whitening, veneers, crowns, and cosmetic bonding, which can address issues such as discoloration, misalignment, and uneven shape.
Smile design can address both aesthetic and functional issues, such as misaligned teeth that can be corrected with orthodontic treatments or aligners.
The duration of the smile design process varies depending on the complexity of the treatment plan, but it typically involves multiple appointments over several weeks or months.
Smile design can also improve oral health by correcting issues such as misaligned teeth that can be difficult to clean, and it can boost confidence in one's appearance.
Yes, smile design can be a significant investment, but many dentists offer financing options and discuss the costs and benefits with patients to help them make an informed decision.
Gum infections can quickly progress from mild discomfort to serious oral health problems if left untreated. Whether you're experiencing swollen, bleeding gums or suspect you might have an infection, understanding effective gum infection treatment options is crucial for preserving your dental health and preventing complications. This guide covers everything from professional treatments to home remedies that can help you address gum infections and restore your oral health.

Visual comparison between healthy gums and infected gums showing key symptoms
Gum infections, also known as periodontal disease, typically begin with bacteria buildup in the mouth. Understanding what causes these infections and recognizing the early warning signs can help you seek timely treatment.
The primary cause of gum infections is poor oral hygiene that allows bacteria to accumulate and form plaque on your teeth. When plaque isn't removed through regular brushing and flossing, it hardens into tartar, which can only be removed by a dental professional.
Identifying the symptoms of a gum infection early can help prevent the condition from worsening. Watch for these warning signs:

Bleeding gums while brushing is a common early sign of gum infection
Don't wait for gum infections to worsen. Early treatment can prevent serious complications and save your natural teeth.
Gum infections progress through several stages, from mild gingivitis to advanced periodontitis. Knowing which stage you're experiencing helps determine the appropriate gum infection treatment.

The progression of periodontal disease from gingivitis to advanced periodontitis
"Gingivitis is the only stage of gum disease that's completely reversible. Once the infection progresses to periodontitis, the damage can be managed but not fully reversed, making early treatment crucial."
When home care isn't enough to address a gum infection, professional dental treatments become necessary. These treatments target the infection at its source and help restore gum health.

Professional scaling and root planing removes bacteria below the gumline
Antibiotics play an important role in treating gum infections, especially when there's active infection present. Your dentist may prescribe:
| Antibiotic Type | Common Uses | Administration |
| Amoxicillin | First-line treatment for many gum infections | Oral tablets or capsules |
| Metronidazole | Targets anaerobic bacteria in periodontal disease | Oral tablets |
| Clindamycin | For severe infections or penicillin allergies | Oral capsules |
| Doxycycline | Low-dose for anti-inflammatory effects | Oral tablets or topical application |
| Chlorhexidine | Controls plaque and gingivitis | Prescription mouthwash |
Important: Antibiotics should only be taken as prescribed by your dentist or doctor. Always complete the full course of antibiotics, even if symptoms improve before you finish.
While professional treatment is essential for moderate to severe gum infections, several home remedies can help manage symptoms and support healing, especially for mild cases.

Natural home remedies can help manage mild gum infection symptoms
A simple saltwater solution can reduce inflammation and kill bacteria. Mix 1/2 teaspoon of salt in a glass of warm water and rinse your mouth for 30 seconds, 2-3 times daily.
Dilute 3% hydrogen peroxide with equal parts water. Swish in your mouth for 30 seconds and spit. This helps reduce bacteria and heal bleeding gums.
Mix 1/4 teaspoon of turmeric powder with a small amount of water to form a paste. Apply to affected gums for 5 minutes, then rinse. Turmeric has natural anti-inflammatory properties.
Add 2-3 drops of tea tree oil to a small amount of water or coconut oil. Apply to gums with a cotton swab. Tea tree oil has antimicrobial properties that fight infection.
Apply pure aloe vera gel directly to inflamed gums. Its anti-inflammatory properties can soothe irritation and promote healing.
Swish 1 tablespoon of coconut or sesame oil in your mouth for 15-20 minutes, then spit it out. This traditional practice may help reduce bacteria and plaque.

Oil pulling with coconut oil can help reduce bacteria that cause gum infections
Remember: Home remedies should complement, not replace, professional dental care. If your symptoms persist for more than 7 days or worsen, consult a dentist immediately.
Home remedies can help with mild symptoms, but a dental professional can provide targeted treatment for your specific condition.
The best treatment for gum infection is prevention. Establishing a consistent oral hygiene routine can significantly reduce your risk of developing gum disease.

Proper brushing and flossing techniques are essential for preventing gum infections

A balanced diet rich in vitamins and minerals supports healthy gums
Pro Tip: Consider using an electric toothbrush, which can be more effective at removing plaque than manual brushing. Many models have built-in timers to ensure you brush for the full recommended two minutes.
While mild gum inflammation might respond to home care, certain symptoms indicate you need professional gum infection treatment right away.

Professional dental examination is crucial when gum infection symptoms are severe
Warning: Untreated gum infections can spread to other parts of your body and may be linked to serious health conditions including heart disease, diabetes complications, respiratory problems, and pregnancy complications. Never ignore persistent gum problems.

Advanced gum infection requiring immediate professional treatment
Treatment time varies depending on the severity of the infection. Mild gingivitis may improve within 10-14 days with proper home care and professional cleaning. Moderate to severe periodontal disease may require multiple treatments over several months, with ongoing maintenance to prevent recurrence.
Most dental insurance plans cover preventive care and basic periodontal treatments like scaling and root planing. Coverage for advanced surgical procedures varies by plan. Check with your insurance provider about specific coverage details and potential out-of-pocket costs.
The bacteria that cause gum infections can be transmitted through saliva. While you can't "catch" periodontal disease directly, the harmful bacteria can be passed between people through kissing or sharing utensils, potentially increasing risk for those with poor oral hygiene or compromised immune systems.
Gum infections can range from mild gingivitis to severe periodontitis, but with proper care and timely treatment, you can restore your gum health and protect your teeth. Remember that early intervention is key—the sooner you address symptoms of gum infection, the better your chances of preventing permanent damage.
Maintaining good oral hygiene, scheduling regular dental check-ups, and addressing risk factors like smoking and diet can significantly reduce your risk of developing gum infections. If you do notice symptoms, don't hesitate to seek professional care while supporting your treatment with appropriate home remedies.

Successful gum infection treatment leads to restored oral health and confidence
Don't let gum infection compromise your oral health and overall wellbeing. Professional treatment can stop the progression of gum disease and help restore your healthy smile.
If your dentist has recommended a root canal treatment, you might feel anxious about what lies ahead. Many patients associate root canals with pain and discomfort, but modern techniques have made this tooth-saving procedure relatively comfortable and straightforward. Understanding the root canal treatment steps can help ease your concerns and prepare you for what to expect. This comprehensive guide walks you through each phase of the procedure, from diagnosis to recovery.

A dentist explaining the root canal treatment process using a dental model
Root canal treatment (also called endodontic therapy) is a dental procedure designed to treat infection at the center of a tooth. The treatment involves removing infected pulp from the tooth's pulp chamber and root canals, cleaning the area, and sealing it to prevent further infection.
Despite its intimidating reputation, root canal therapy is actually a pain-relieving procedure. The discomfort many associate with root canals typically comes from the infection itself, not the treatment. Modern techniques and effective anesthesia make the procedure comparable to receiving a routine filling.

Anatomy of a tooth showing the pulp chamber and root canals that require treatment
"Root canal treatment doesn't cause pain, it relieves it. The procedure is similar to having a deep filling placed, and modern techniques have made it much more comfortable than in the past."
Before beginning the root canal procedure, your dentist will conduct a thorough examination of the affected tooth and surrounding tissues. This typically includes:
This diagnostic phase usually takes 15-30 minutes and helps your dentist develop a precise treatment plan tailored to your specific needs.

Dental X-ray revealing infection in the root canal requiring treatment
To ensure your comfort during the procedure, your dentist will administer local anesthesia to numb the affected tooth and surrounding area. This step involves:
You'll remain awake during the procedure, but the treatment area will be completely numb. Many dentists also offer additional comfort options like nitrous oxide (laughing gas) for patients with dental anxiety.

Administration of local anesthesia ensures a pain-free root canal procedure
Once the area is completely numb, your dentist will:
This phase typically takes 10-15 minutes and is similar to the preparation for a deep filling. The dental dam is essential as it prevents saliva and bacteria from contaminating the treatment area.

Dental dam isolation keeps the tooth clean and dry during treatment
This critical phase involves removing the infected pulp and preparing the canals for filling:
This is typically the longest part of the procedure, taking 30-60 minutes depending on the tooth's complexity. Molars with multiple canals require more time than front teeth with single canals.

Specialized endodontic files clean and shape the root canals
After thoroughly cleaning and shaping the canals, your dentist will:
This filling process typically takes 15-30 minutes. Gutta-percha is the standard filling material because it's flexible, biocompatible, and can be heated and compressed to fit the canal precisely.

Gutta-percha filling material seals the cleaned root canals
After filling the root canals, your dentist will:
This step takes approximately 15-20 minutes. If your treatment requires multiple visits, a temporary filling will protect the tooth between appointments. For single-visit procedures, a permanent filling may be placed immediately.

Placement of a filling to seal the access hole after root canal treatment
In many cases, especially for back teeth, a crown is recommended after root canal treatment:
Crown placement typically occurs 1-2 weeks after the root canal procedure and takes about 30-60 minutes. Crowns provide crucial protection for teeth that have undergone root canal treatment, preventing fractures and ensuring long-term success.

Before and after crown placement following root canal treatment
Some discomfort is normal for a few days after treatment. Most patients manage well with these strategies:
Contact your dentist if pain is severe or persists beyond a few days, as this could indicate a complication requiring attention.
While your tooth heals, especially if you have a temporary filling or crown, be cautious with your diet:
Soft foods like yogurt, smoothies, pasta, and eggs are ideal during the initial recovery period.

Soft foods recommended during recovery after root canal treatment
Modern root canal treatment is not significantly more painful than having a filling placed. The area is thoroughly numbed before the procedure begins, and most patients report feeling pressure but not pain during treatment. The discomfort many associate with root canals typically comes from the infection itself, not the procedure that relieves it. Most patients experience mild to moderate discomfort for a few days after treatment, which can be managed with over-the-counter pain medications.
Most patients can return to normal activities the day after root canal treatment. The initial tenderness and sensitivity typically subside within a few days to a week. Complete healing of the tissues around the root may take several weeks, but this doesn't usually cause noticeable symptoms. If you received a temporary filling, you'll need to be careful with that tooth until your permanent restoration is placed, which usually occurs within 1-2 weeks after the root canal procedure.
A typical root canal treatment takes between 60-90 minutes for a single appointment. Simple cases involving front teeth with single canals may be completed in under an hour. More complex cases involving molars with multiple canals might take longer or require multiple appointments. Your dentist will provide a time estimate based on your specific situation during your consultation.
In most cases, yes—especially for premolars and molars. After root canal treatment, teeth become more brittle and susceptible to fracture. A crown provides crucial protection by encasing the entire visible portion of the tooth above the gumline. Front teeth that undergo root canal treatment may not always require crowns if they have sufficient remaining healthy tooth structure and aren't subject to heavy biting forces.
Root canal treatment is a highly effective procedure that can save your natural tooth and relieve pain caused by infection or damage. Modern techniques have made the process more comfortable and efficient than ever before. By understanding the root canal treatment steps outlined in this guide, you can approach your procedure with confidence rather than anxiety.
Remember that preserving your natural teeth whenever possible is always preferable to extraction. A tooth that has undergone successful root canal therapy can last a lifetime with proper care and regular dental check-ups.
If you're experiencing tooth pain or have been told you need a root canal, consulting with a qualified dentist is the best next step. A professional evaluation will determine if root canal treatment is right for you and help preserve your natural smile.

A healthy, natural smile preserved through successful root canal treatment
Proper after tooth extraction care is crucial for a smooth recovery and preventing complications. Whether you've had a wisdom tooth removed or another dental extraction, following the right aftercare procedures helps ensure proper healing, reduces discomfort, and prevents issues like dry socket or infection. This comprehensive guide covers everything you need to know about caring for your mouth after a tooth extraction.
The first 24 hours following your tooth extraction are critical for proper healing. During this time, a blood clot forms in the socket where your tooth was removed. This clot is essential for the healing process and must be protected.

Immediately after your procedure, your dentist will place gauze over the extraction site. Here's how to manage this crucial first step:
Your body position can impact healing and comfort levels after an extraction:
Some discomfort and swelling are normal after a tooth extraction. Effective management of these symptoms can make your recovery much more comfortable.

Cold therapy is highly effective for reducing swelling and numbing pain:
Your dentist may prescribe pain medication, but over-the-counter options can also be effective:
If you're experiencing severe pain that isn't controlled by your prescribed medications, contact your dental provider immediately as this could indicate a complication.
The first two days after your tooth extraction are crucial for proper healing. Following these guidelines will help protect the blood clot and promote recovery.

What you eat and drink can significantly impact your healing process:
Certain activities can disrupt the blood clot and delay healing:

Keeping your mouth clean is essential for preventing infection, but you must be gentle around the extraction site. Follow these guidelines for proper oral hygiene during recovery.

You can continue brushing your teeth after an extraction, but with some modifications:
After the first 24 hours, salt water rinses can help keep the area clean:
While most tooth extractions heal without issues, it's important to recognize the signs of potential complications that require professional attention.

Dry socket occurs when the blood clot is dislodged or dissolves before healing is complete. This painful condition typically develops 3-5 days after extraction.
While some swelling is normal after an extraction, these symptoms may indicate an infection:
If you notice any signs of dry socket or infection, contact your dental provider immediately. Prompt treatment can prevent more serious complications.
Understanding what to expect during each phase of healing can help you monitor your progress and know when you're on track.

| Time Period | What to Expect | Care Focus |
| First 24 Hours | Blood clot formation, bleeding, swelling begins | Gauze pressure, ice packs, rest, avoid disturbing clot |
| 24-72 Hours | Peak swelling, decreasing pain, clot stabilizing | Salt water rinses, soft foods, gentle oral hygiene |
| 3-7 Days | Swelling subsides, gum tissue begins healing | Continued gentle care, gradually returning to normal diet |
| 1-2 Weeks | Soft tissue healing, socket filling in | Normal oral hygiene, avoiding hard foods at extraction site |
| 3-4 Weeks | Socket continues filling with new tissue | Return to normal activities and diet |
| 1-3 Months | Bone remodeling continues beneath the surface | Regular dental hygiene, follow-up with dentist if needed |
Here are answers to common questions patients have about the tooth extraction recovery process.

Some bleeding is normal for the first 24 hours after an extraction. Active bleeding should slow significantly within a few hours. You may notice pink or blood-tinged saliva for up to 48 hours. If you experience heavy bleeding that doesn't stop after applying pressure with gauze for 30-45 minutes, contact your dental provider.
You should avoid smoking and alcohol for at least 72 hours (3 days) after an extraction, though waiting a full week is ideal. Smoking significantly increases the risk of dry socket by reducing blood supply to the healing area and introducing suction that can dislodge the blood clot. Alcohol can interfere with blood clotting, delay healing, and may interact with prescribed medications.
The timeline varies depending on the complexity of the extraction and individual factors. Soft tissue typically heals within 1-2 weeks. The socket will gradually fill in with new tissue over 3-4 weeks. Complete bone healing and remodeling can take 3-6 months, though this occurs beneath the surface and doesn't affect your comfort or function after the initial healing period.
Avoid strenuous physical activity for at least 24-48 hours after an extraction. Elevated heart rate and blood pressure can increase bleeding and discomfort. Light activities can usually be resumed after 2 days, but wait at least 3-4 days before returning to vigorous exercise, heavy lifting, or sports. Always follow your dentist's specific recommendations based on your extraction.
Some degree of bad breath is normal during the healing process, especially in the first week. This occurs due to blood in the mouth, reduced ability to clean thoroughly, and the healing process itself. However, persistent or worsening bad breath accompanied by a foul taste may indicate an infection and should be evaluated by your dentist.
Proper after tooth extraction care is essential for a smooth recovery and preventing complications. By following the guidelines in this guide—protecting the blood clot, managing pain and swelling, maintaining gentle oral hygiene, and watching for warning signs—you can help ensure optimal healing after your procedure.

Remember that everyone's healing process is unique, and factors like the complexity of your extraction, your overall health, and how closely you follow aftercare instructions can all impact your recovery timeline. When in doubt, always contact your dental provider with questions or concerns.
If you're experiencing complications after a tooth extraction or have questions about your recovery, don't hesitate to seek professional dental care. Prompt attention can prevent more serious issues and ensure proper healing.
A toothache can range from a mild annoyance to debilitating pain that disrupts your daily life. Understanding the underlying causes of tooth pain is the first step toward finding relief. Whether you're experiencing sharp, throbbing pain or a dull ache that won't go away, this comprehensive guide explores the common triggers of toothaches and when you should seek professional dental care.

Cross-section of a tooth showing the key anatomical structures involved in toothache
To understand what causes toothache, it's helpful to know the basic structure of a tooth. Each tooth consists of several layers:
When any part of this structure is damaged or infected, the nerves in the pulp can become irritated, resulting in the pain we recognize as a toothache. Now, let's explore the most common causes of this discomfort.

The most frequent cause of toothache is dental decay. When bacteria in your mouth produce acids that eat away at your tooth enamel, cavities form. As decay progresses deeper into the tooth, it can reach the dentin and eventually the pulp, causing pain that ranges from mild sensitivity to severe throbbing.
An abscess is a pocket of infection at the root of a tooth or in the surrounding gum tissue. This serious condition occurs when bacteria invade the pulp chamber, causing inflammation, tissue death, and pus accumulation. Symptoms include severe, throbbing pain, swelling, fever, and a foul taste in your mouth. An abscess requires immediate professional treatment.
Warning: If you experience severe throbbing pain along with fever, facial swelling, or difficulty swallowing, seek emergency dental care immediately. A dental abscess can lead to serious complications if left untreated.

Teeth can crack or fracture from trauma, biting hard objects, or even normal wear and tear. When a crack extends into the pulp, it can cause significant pain, especially when chewing or exposed to temperature changes. Some cracks may be invisible to the naked eye but can still cause considerable discomfort.
Gingivitis and more advanced periodontitis affect the tissues surrounding your teeth. As gum disease progresses, it can cause the gums to pull away from teeth, creating pockets where bacteria thrive. This infection can lead to inflammation, bone loss, and tooth pain. Signs include bleeding gums, bad breath, and tender, swollen gum tissue around teeth.
Gum recession can expose the roots of your teeth, which aren't protected by enamel. These exposed roots are highly sensitive to temperature changes, acidic foods, and even touch. This condition, known as dentin hypersensitivity, can cause sharp, temporary pain when triggered.

Over time, dental fillings, crowns, or other restorations can wear down, crack, or become loose. When this happens, the protective seal is broken, allowing bacteria to enter and potentially cause decay beneath the restoration. This can result in sensitivity and pain, particularly when chewing or exposed to temperature changes.
When wisdom teeth (third molars) don't have enough room to emerge properly, they can become impacted. This can cause pressure, pain, and inflammation in the surrounding tissues. Sometimes, partially erupted wisdom teeth create spaces where bacteria can enter, leading to infection and pain.
Impacted wisdom teeth require professional evaluation. Our dental specialists can assess your situation and recommend appropriate treatment.

Bruxism refers to unconsciously grinding or clenching your teeth, often during sleep. This habit puts excessive pressure on teeth and can lead to worn enamel, fractured teeth, and jaw pain. Many people with bruxism experience dull headaches and sore jaw muscles upon waking.
When baby teeth emerge through the gums (teething) or when permanent teeth replace baby teeth, children often experience discomfort or pain. This is a normal part of development but can cause temporary toothaches as the teeth push through the gums.
After braces are tightened or adjusted, teeth may become sore for a few days. This temporary pain occurs as teeth begin to move into their new positions and is typically mild to moderate.
Pulpitis is inflammation of the pulp tissue inside the tooth. It can be reversible (mild inflammation that resolves with treatment) or irreversible (severe inflammation requiring root canal therapy). Symptoms include pain when eating hot, cold, or sweet foods that lingers even after the stimulus is removed.

Direct impact to the mouth from falls, sports injuries, or accidents can damage teeth and surrounding tissues. Even if a tooth doesn't appear broken, trauma can cause internal damage to the pulp, resulting in pain and sensitivity.
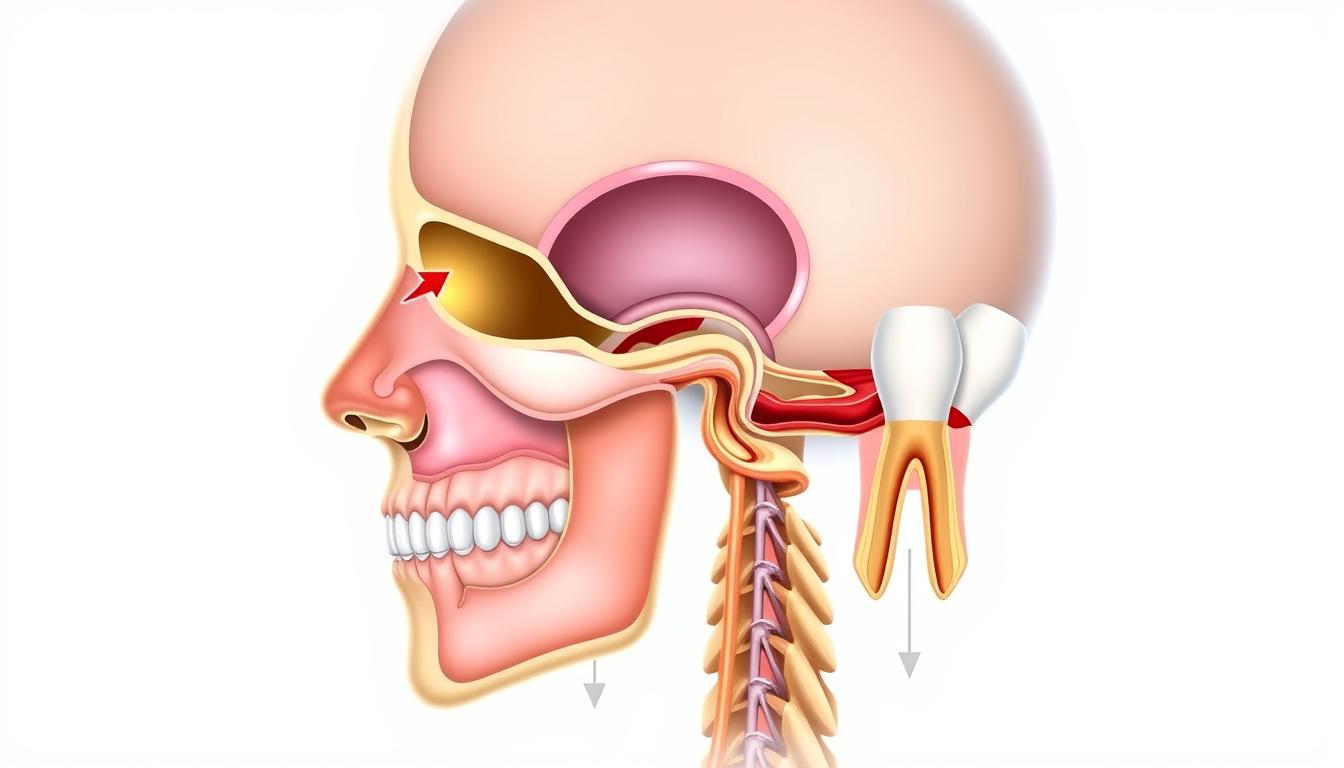
The roots of your upper molars are located close to your maxillary sinuses. When these sinuses become infected or inflamed, the pressure can cause pain that feels like it's coming from your teeth. This type of toothache often affects multiple upper teeth and may worsen when bending over or lying down.
The temporomandibular joint (TMJ) connects your jawbone to your skull. Disorders affecting this joint can cause pain that radiates to your teeth, making it feel like a toothache. Other symptoms include jaw clicking, difficulty opening your mouth fully, and facial pain.
This chronic pain condition affects the trigeminal nerve, which carries sensation from your face to your brain. Trigeminal neuralgia can cause intense, electric-shock-like pain that may be mistaken for a toothache. The pain is typically triggered by normal activities like eating, talking, or brushing teeth.
Important: In rare cases, tooth pain—particularly in the lower left jaw—can be referred pain from the heart. If you experience tooth or jaw pain along with chest discomfort, shortness of breath, nausea, or sweating, seek emergency medical attention immediately.
Psychological stress can manifest physically in various ways, including tooth pain. Stress may lead to increased muscle tension in the jaw, bruxism, or changes in pain perception that make existing dental issues feel more severe.

While some mild toothaches can be temporarily managed at home, certain symptoms indicate a serious problem requiring prompt professional attention. Seek immediate dental care if you experience:
Don't wait until it's too late. Dental emergencies require prompt attention to prevent complications and relieve pain.
While waiting to see a dentist, these measures may provide temporary relief:
Remember: These measures provide only temporary relief and are not substitutes for professional dental treatment. The underlying cause of your toothache still needs to be addressed by a dentist.

Many toothaches can be prevented with proper dental hygiene and regular professional care:
Regular dental visits are essential for preventing toothaches and maintaining oral health. Schedule your appointment today.
Yes, stress can indirectly cause tooth pain through several mechanisms. When stressed, many people unconsciously clench or grind their teeth (bruxism), which can lead to worn enamel, tooth sensitivity, and jaw pain. Stress can also weaken your immune system, making you more susceptible to infections, including those affecting your teeth and gums. Additionally, stress may cause you to neglect oral hygiene routines, potentially leading to decay and gum problems.
Toothaches often intensify at night for several reasons. When you lie down, blood pressure to your head increases, which can enhance pain sensation in an already inflamed tooth. Additionally, there are fewer distractions at night, making you more aware of the pain. Some people also grind their teeth during sleep, aggravating existing dental issues. The reduced saliva production during sleep also means less natural cleansing and buffering of the mouth, potentially worsening inflammation.
Minor tooth sensitivity or irritation may occasionally resolve on its own, particularly if it's caused by temporary gum irritation or minor trauma. However, most true toothaches are symptoms of underlying conditions like decay, infection, or structural damage that will not improve without treatment. In fact, dental problems typically worsen over time if left untreated, potentially leading to more severe pain, infection, and tooth loss. Even if pain subsides temporarily, the underlying issue likely remains and requires professional attention.
Consider your toothache potentially serious if you experience: severe pain that interferes with daily activities or sleep; pain lasting longer than 1-2 days; swelling in your face, jaw, or gums; fever or chills; difficulty swallowing or breathing; pain when biting down; extremely sensitive teeth; or a foul taste/odor from the affected area. These symptoms may indicate infection, abscess, or other conditions requiring prompt professional treatment. When in doubt, it's always safer to consult a dental professional.
Pain triggered by sweet foods often indicates exposed dentin, the layer beneath your tooth's enamel. This exposure can result from enamel erosion, receding gums, or developing cavities. When sugar contacts exposed dentin, it creates an osmotic pressure change that stimulates the nerve endings, causing pain. This symptom is common in early-stage cavities and should prompt a dental visit, as it suggests your tooth's protective layers have been compromised.

Toothaches can significantly impact your quality of life, but understanding their causes is the first step toward finding relief. While temporary measures may provide short-term comfort, addressing the underlying issue is essential for long-term oral health.
Remember that many dental problems worsen over time if left untreated. What begins as a minor cavity can progress to severe infection, potentially leading to tooth loss and more serious health complications. Regular dental check-ups, good oral hygiene practices, and prompt attention to dental concerns are your best defenses against toothaches.
If you're experiencing tooth pain, don't hesitate to seek professional dental care. Your dentist can accurately diagnose the cause of your discomfort and recommend appropriate treatment to restore your oral health and comfort.
Our dental professionals are ready to help diagnose and treat the cause of your toothache. Take the first step toward relief today.
As England's football captain and Tottenham's all-time leading scorer, Harry Kane has made a lasting impact on the sport. Fans admire his skill, dedication, and leadership on the field. But alongside his athletic success, many have noticed changes in his appearance over the years.
Public interest in his physical transformation has grown, particularly regarding his hair. Observers have noted a shift in his hairline, with some speculating about possible restoration treatments. This article examines the changes while exploring solutions for those facing similar concerns.
Experts classify his hair loss pattern as Norwood Level 2, characterized by an M-shaped recession. Understanding these changes helps shed light on available options for maintaining a confident appearance throughout one's career.
Male pattern baldness affects millions, and even elite athletes aren’t immune to its effects. By 2014, subtle changes in the footballer’s hairline became noticeable, particularly at the temples. This progression aligns with the Norwood Scale’s Stage 2 classification, where recession forms an M-shape.
Photos from 2011 to 2014 reveal gradual thinning at the crown and temples. The hormone DHT shrinks follicles in genetically sensitive areas, causing strands to weaken over years. By age 30, 50% of men experience this pattern.
Fans and media often spotlight appearance shifts, adding pressure.
"Athletes face unique stress when physical changes become public discourse,"
notes a sports psychologist. Hereditary factors also play a role—similar widow’s peaks appear in relatives.
For Norwood Stage 2, recession typically advances over 6–12 years. Modern treatments, however, offer solutions to restore confidence.

The Norwood Scale provides a clear framework for classifying hair loss patterns, from subtle recession to advanced thinning. This system helps identify stages like the footballer’s Norwood Level 2, where temples recede into an M-shape. Early detection allows for tailored treatments to slow progression.
DHT (dihydrotestosterone) binds to androgen receptors in scalp tissue, shrinking follicles over time. This hormone primarily affects the crown and temples, where genetically sensitive hair weakens. By disrupting growth cycles, DHT causes strands to become finer until they stop regenerating.
Frontal and crown thinning often occur together, though mid-scalp regions may remain stable longer. This explains why some men retain density at the top while temples recede visibly.
Stage 2 on the Norwood scale marks the first visible signs of a receding hairline. Compared to advanced stages, it shows:
Staging helps experts recommend interventions, from topical treatments to transplants. For public figures, early action can preserve both hair and confidence under scrutiny.
The question of whether a high-profile footballer underwent a hair transplant has drawn significant attention. While no official confirmation exists, experts and fans scrutinize visual evidence for clues.
High-resolution comparisons of 2018 and 2023 photos reveal minimal temple restoration. Advanced techniques like unshaven FUE allow discreet procedures without shaving the entire scalp. This could explain the lack of obvious surgical signs.
Clinics note that "anchored grafts" blend naturally with existing hair. However, styling products and strategic haircuts may also create the illusion of fuller results. Wayne Rooney’s confirmed transplant serves as a benchmark for detectable changes.
Key observations from 4K magnification analysis include:
Unlike Rooney’s dramatic transformation, the footballer’s case leans toward conservative grooming choices. For public figures, even minor adjustments spark speculation about hair transplant procedures.
Follicular Unit Extraction (FUE) has become the gold standard for surgical hair restoration. This minimally invasive process extracts individual grafts from the back of the head, where hair is genetically resistant to thinning. Unlike older methods, FUE leaves no linear scars, making it ideal for active lifestyles.
Using micro-punches as small as 0.8mm, surgeons harvest DHT-resistant follicles from the occipital zone. These grafts, each containing 1–4 hairs, are then implanted into thinning areas. Advanced robotic systems map the "safe donor area" along the lateral humps for optimal yield.
Key advantages include:
Follicles from the donor zone lack sensitivity to DHT, the hormone causing pattern baldness.
"These follicles maintain their growth cycle even after transplant,"
explains a leading trichologist. Over 12–15 months, transplanted hair thickens, blending seamlessly with existing strands.
Compared to FUT (strip harvesting), FUE’s precision reduces trauma, ensuring faster healing. For public figures, this discreet process avoids abrupt changes that draw scrutiny.
Modern hair restoration techniques offer transformative solutions for athletes concerned about receding hairlines. These procedures can recreate natural hairlines while maintaining the active lifestyles required in competitive sports.
For Norwood Stage 2 patterns, approximately 1700 grafts typically reconstruct temporal peaks. Surgeons distribute follicles strategically across the frontal area to:
A 32-year-old case study with identical hair loss showed 82% density improvement after FUE. This matches what athletes could expect when they get hair transplant procedures.
Advanced techniques ensure transplanted hair blends seamlessly with existing strands.
"The goal is undetectable restoration that withstands close-up scrutiny,"
explains a leading surgeon.
For sports professionals, a specialized 7-day protocol includes:
Maintenance options like minoxidil or SMP touch-ups preserve the look long-term. With proper care, results typically last 10-20 years - covering most athletic careers.
Public figures face unique pressures when it comes to appearance, especially in the spotlight of professional sports. For many celebrities, hair restoration isn’t just about vanity—it’s a career investment. The rise in procedures among high-profile men reflects this shift.
Wayne Rooney’s £30,000 transplant at age 25 set a precedent for football stars. Over eight years, his three-stage journey restored a receding hairline to near-original density. Clinics now use his case to showcase modern techniques.
Rooney’s openness sparked a trend. Media training, like Antonio Conte’s post-op strategy, helps people manage public reactions. His results prove transplants can look natural under scrutiny.
Studies link fuller hair to perceived leadership competence. A 72% surge in male celebrities opting for procedures (2010–2020) highlights this bias. For athletes, maintaining a youthful image often aligns with sponsorship deals.
| Factor | UK Clinics | Turkey Clinics |
|---|---|---|
| Average Cost | £5,000–£15,000 | £1,500–£3,500 |
| Recovery Time | 7–10 days | 5–7 days |
| Celebrity Clients | 35% | 65% |
Five footballers who confirmed transplants include:
For public figures, the decision blends personal confidence with professional branding. The results speak for themselves.
Hair restoration procedures vary widely in price based on multiple factors. Understanding these variables helps set realistic budgets for those considering treatment. The investment often proves worthwhile for long-term confidence and appearance.
Surgeon expertise accounts for 40-60% of total cost. Board-certified specialists with proven results typically charge premium rates. Clinic location also plays a major role, with urban centers demanding higher fees than rural practices.
Additional price determinants include:
The number of many grafts needed directly impacts the final price. Norwood Stage 2 cases typically require 1800-2200 grafts for optimal coverage. Each graft contains 1-4 hairs, with pricing usually calculated per unit.
Here's how costs compare across regions:
| Location | Price Per Graft | Total for 2000 Grafts |
|---|---|---|
| United Kingdom | £3.50-£7 | £7,000-£14,000 |
| Western Europe | £2.10-£3.50 | £4,200-£7,000 |
| Eastern Europe | £1.20-£2.80 | £2,400-£5,600 |
Several clinics offer finance options to make procedures more accessible. Popular plans include:
Most providers offer free consultations with detailed cost breakdowns. This transparency helps patients make informed decisions about their hair restoration journey.
For those hesitant about surgical options, effective non-surgical treatments exist for hair loss. These solutions range from medical therapies to cosmetic camouflage techniques. Many patients achieve noticeable results without going under the knife.
Topical finasteride shows 86% efficacy in clinical trials with fewer side effects than oral versions. This treatment blocks DHT, the hormone responsible for pattern baldness. Unlike pills, the topical form minimizes systemic absorption.
Low-level laser therapy (LLLT) helmets demonstrate promise for early-stage thinning. Regular use stimulates follicles to prolong growth cycles. Most users see results within 3-6 months of consistent treatment.
Platelet-rich plasma (PRP) injections with ultrasound guidance boost natural regrowth. This procedure concentrates healing factors from your own blood. Many clinics recommend 3-4 sessions spaced six weeks apart for optimal results.
A textured crop hairstyle creates the illusion of fuller coverage. This look works well for receding hairlines and diffuse thinning. Strategic layering adds volume while disguising sparse areas.
Keratin fiber concealers provide instant density without commitment. These charged particles cling to existing strands, blending seamlessly. For longer-lasting solutions, semi-permanent tint sprays match natural hair color.
Micropigmentation offers a 4-7 year solution for significant loss. This technique tattoos tiny dots that mimic shaved hair follicles. It's particularly effective for creating defined hairlines and adding density.
With these alternatives, patients can get hair solutions tailored to their needs and comfort levels. The right approach depends on individual patterns and desired outcomes.
Confidence in appearance significantly impacts professional success and personal well-being. A 2023 YouGov survey found 68% of people believe hair loss affected their career progression. This perception stems from societal associations between full hair and vitality.
fMRI studies reveal surprising neurological effects. Participants viewing restored hairlines rated individuals 5-7 years younger than their actual age. This youth perception bias influences hiring decisions and leadership assessments.
Male-dominated professions show higher rates of body dysmorphia related to hair loss. Among men in sales and executive roles, 42% report avoiding social situations during progressive thinning phases.
"Endorsement deals increased 300% post-restoration for some athletes,"
This commercial benefit explains why 94% of transplant recipients report improved quality of life. The transformation extends beyond physical changes to self-confidence in professional settings.
Medical and surgical approaches yield different psychological outcomes:
Public figure transparency has reduced stigma significantly. When high-profile individuals share restoration journeys, it normalizes the process for everyday professionals. The right look can become a career asset rather than a source of anxiety.
Taking control of hair loss starts with understanding your options. Early intervention yields the best results, especially for those at Norwood Stage 2. A 2200-graft procedure could restore density while maintaining a natural look.
Top UK clinics like The Treatment Rooms (020 8706 0076) offer personalized plans. Their expert team ensures high success rates, backed by guarantees like HairPalace’s 80% growth promise. Comparing accredited providers helps you make an informed choice.
Whether you get hair transplant solutions or explore non-surgical treatments, acting today preserves more follicles. Confidence in your appearance impacts both personal and professional life. Start your hair restoration journey now for lasting results.
Thinning at the temples, a receding hairline, and gradual loss at the crown are common early indicators. These changes often follow the Norwood Scale progression.
While he hasn’t confirmed it, side-by-side comparisons suggest significant restoration, particularly in the hairline and temple areas—consistent with FUE transplant results.
Follicular Unit Extraction (FUE) involves harvesting individual grafts from donor areas (typically the back of the head) and implanting them in thinning zones. The method ensures minimal scarring and natural regrowth.
Donor hairs are genetically resistant to DHT, the hormone causing male pattern baldness. Transplanted grafts retain this trait, offering permanent results.
Prices vary by graft count, clinic reputation, and location. Procedures can range from ,000 to ,000, with personalized estimates after consultation.
Yes. Treatments like minoxidil, finasteride, and PRP therapy can slow loss or stimulate growth, while strategic styling and fibers offer temporary cosmetic improvements.
Initial healing takes 7–10 days, with full results visible after 12–18 months as transplanted hairs grow naturally.
Public figures often seek restoration to maintain a youthful image, boost confidence, and counteract the psychological impact of hair loss under constant media scrutiny.